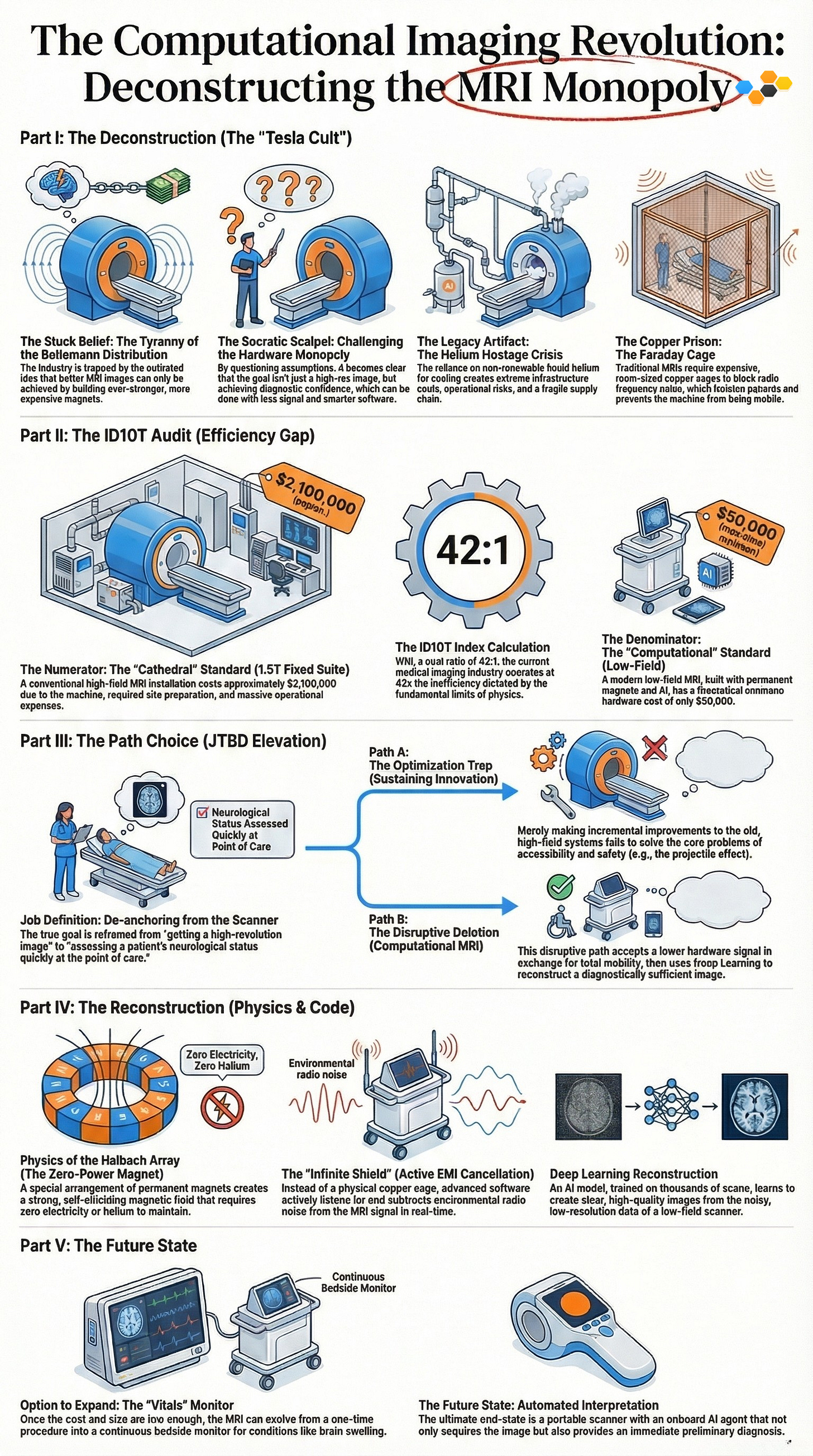
The medical imaging industry is stuck building massive, expensive "Cathedrals" for MRI machines because they believe better images only come from giant magnets. This old-fashioned thinking makes current scanners 42 times more expensive than necessary, costing millions for hardware when physics says it should cost about $50,000. By replacing expensive copper shielding and super-cold magnets with smart software and artificial intelligence, we can build portable, affordable scanners that plug into a regular wall outlet. This shift turns MRI from a rare, expensive procedure into a common tool that doctors can bring directly to the patient's bedside to diagnose strokes instantly.
Executive Summary: The End of the “Cathedral” Model
Audience: Healthcare Strategists, Hardware Engineers, Deep Tech Investors
The medical imaging industry is currently trapped in a “Hardware Arms Race,” operating on the flawed, linear assumption that diagnostic utility is strictly a function of magnetic field strength …
This “Reasoning by Analogy” has produced 7-Tesla “Cathedrals”—immensely expensive, immovable suites requiring liquid helium cooling—that alienate patients from care.
This document deconstructs that monopoly. By applying First Principles thinking, we demonstrate that Signal-to-Noise Ratio (SNR) is no longer solely a hardware constraint (Atoms) but a computational one (Bits). The convergence of low-field permanent magnet physics (0.064T), active electromagnetic interference cancellation, and Deep Learning reconstruction (DL-ESPIRiT) enables a scanner with a Theoretical Minimum Cost of ~$50,000 to perform the same Job-to-be-Done as a $2.1 million machine: detecting pathology at the point of care. We are witnessing the shift from MRI as a procedure to MRI as a utility.
Part I: The Deconstruction (The “Tesla Cult”)
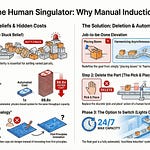
The Stuck Belief: The Tyranny of the Boltzmann Distribution
The central dogma of modern radiology is that Image Quality is a function of Magnetic Field Strength. To understand why the industry is stuck, we must understand the physics they are optimizing for.
MRI works by aligning the protons of hydrogen atoms (mostly in water) with a magnetic field. The clarity of the image depends on how many protons align “up” versus “down.” The ratio of this alignment is governed by the Boltzmann Distribution:
Where…
(the energy difference) is directly proportional to the magnetic field strength.
The Industry Logic: To get more signal (higher SNR), you simply increase magnetic field strenght.
The Consequence: This created a linear innovation trajectory.
\(0.5T \rightarrow 1.5T \rightarrow 3.0T \rightarrow 7.0T\)The Cost Function: While Signal scales roughly linearly with Field Strength, Cost scales quadratically (or exponentially) due to the requirements of superconductivity.
This logic is a classic “Reasoning by Analogy” trap. It assumes that the only way to recover structure from data is to increase the volume of the raw signal. In the pre-GPU era, this was true. In the post-Transformer era, it is false. We are effectively paying millions of dollars for “Hardware SNR” when “Software SNR” (reconstruction algorithms) costs pennies per inference.
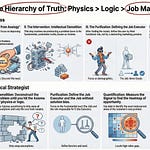
The Socratic Scalpel: Challenging the Hardware Monopoly
We must apply the Socratic Inquiry to dismantle the “High-Field” consensus.
Inquiry 1 (Clarification): “What exactly are we buying when we spend $2 million on a 3T magnet?”
The Surface Answer: “We are buying high-resolution images.”
The First Principles Answer: “No. We are buying proton alignment. We are buying a higher probability that a hydrogen nucleus will precess at the Larmor frequency in a detectible way.”
Inquiry 2 (Challenging Assumptions): “Why must signal alignment be physical? Is it possible to reconstruct the structure of the anatomy from a lower signal using probabilistic models?”
The Assumption: “You cannot image what you cannot measure.”
The Counter-Evidence: Modern Deep Learning models (U-Nets, GANs) routinely upscale 480p video to 4K. The “texture” of high resolution can be hallucinated mathematically if the underlying “structure” (anatomy) is preserved.
Inquiry 3 (Implication): “If diagnostic confidence can be achieved at 64mT (milliTesla), what happens to the infrastructure?”
The Result: If we drop the field strength, we lose the requirement for superconductivity. If we lose superconductivity, we lose Liquid Helium. If we lose Liquid Helium, the scanner becomes a consumer appliance.
The Legacy Artifact: The Helium Hostage Crisis
The single greatest barrier to MRI accessibility is Liquid Helium. To maintain a superconducting magnet, the coils must be bathed in liquid helium to reach 4 Kelvin (-452°F). This creates a cascade of physical constraints that define the “Cathedral” model.
The Quench Pipe (Infrastructure Cost)
If a superconducting magnet loses its cooling (a “quench”), the liquid helium boils instantly, expanding 700:1 in volume.
The Constraint: This requires massive, dedicated cryogenic exhaust pipes (typically 10-12 inch diameter stainless steel) routed directly to the outside of the building.
The Cost: Retrofitting a hospital room with quench pipes typically costs $50,000 - $150,000 alone. This makes mobile deployment impossible; you cannot attach a quench pipe to an elevator.
The Supply Chain Shock (Operational Risk)
Helium is a non-renewable resource, typically a byproduct of natural gas extraction.
Source Concentration: The majority of the world’s supply comes from the US (Cliffside Field), Qatar, and Russia.
Volatility: Prices have quadrupled in the last decade. Hospitals are frequently placed on “allocation,” meaning they cannot top off their scanners, risking a catastrophic quench.
Conclusion: Building a global healthcare infrastructure on a volatile, non-renewable noble gas is a strategic failure. The cooling system is not a feature; it is a Process Artifact.
The Copper Prison: The Faraday Cage
High-field MRI systems operate at Larmor frequencies that overlap with commercial FM radio (64 MHz at 1.5T). Because the MRI signal is radio-frequency (RF), external radio waves will ruin the image.
The Legacy Solution: Build a Faraday Cage. A room completely lined with copper shielding.
The Cost: Shielding a standard MRI suite requires tons of copper and specialized labor, costing $30,000 - $50,000.
The Isolation: This cage physically separates the patient from the rest of the ICU. You cannot simply roll a 1.5T scanner next to a ventilator because the ventilator is an RF noise source, and the scanner is an RF receiver. The cage is a “monument to passive engineering.”
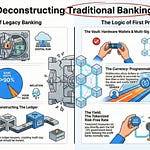
Part II: The ID10T Audit (Efficiency Gap)
To quantify the inefficiency of the current model, we apply the ID10T Index (Inefficiency Delta in Operational Transformation). We compare the Current Commercial Price of the status quo against the Theoretical Minimum Cost dictated by physics.
The Numerator: The “Cathedral” Standard (1.5T Fixed Suite)
The cost of a standard installation is driven by weight, power, and shielding requirements. These are not “medical” costs; they are “physics management” costs.
Hardware (The Machine): ~$1,500,000.
Superconducting Niobium-Titanium coils.
Cryostats.
High-voltage gradient amplifiers (2000V+).
Site Preparation (The Room): ~$500,000.
Copper Faraday Cage.
Structural reinforcement (floor loading for 5+ tons).
Cryogen exhaust venting (Quench pipe).
Magnetic shielding (Silicon steel to contain the 5-Gauss line).
Operational Opex (The Tax): ~$100,000/year.
Helium top-offs.
Cold-head replacement (mechanical cryocooler).
Electricity (50-100 kW peak power draw).
Total Numerator: ~$2,100,000 + Strict Zoning.
The Denominator: The “Computational” Standard (Low-Field)
The theoretical minimum cost relies on Permanent Magnets (which require zero power) and Compute (which rides Moore’s Law).
Atoms (The Magnet): ~$15,000.
Material: Sintered Neodymium-Iron-Boron (NdFeB), Grade N48 or N52.
Configuration: Halbach Array (Self-shielding).
Mass: ~300kg.
Calculation: 300kg $\times$ ~$50/kg (Spot Price) = $15,000.
Bits (The Shield & Reconstruction): ~$1,000.
EMI Sensors: Standard RF antennas (<$100).
Compute: NVIDIA Jetson or similar edge inference module (<$1,000).
Reconstruction Cost: ~$0.10 per scan (Energy cost of inference).
Regulatory Floor: ~$75/hr.
Operated by an L2 Skilled Tech or Nurse, rather than an L3 Specialist.
Total Denominator: ~$50,000 Hardware Cost.
The ID10T Index Calculation
The Verdict: The medical imaging industry is operating at 42x inefficiency. It’s clearly not the answer to Life, the Universe, and Everything.
We are paying for Passive Shielding (Copper) instead of Active Cancellation (Algorithms).
We are paying for Hardware Signal (Superconductors) instead of Software Signal (Deep Learning).
Every dollar spent above $50k is a subsidy for “Reasoning by Analogy.”
Part III: The Path Choice (JTBD Elevation)
Innovation requires elevating the Job-to-be-Done (JTBD) to a level of abstraction that allows for disruptive solutions. We must define the job in terms of the patient’s struggle, not the machine’s capability.
Job Definition: De-anchoring from the Scanner
Level 1 (The Trap): “Generating a high-resolution T1-weighted image of the brain.”
Why it fails: This job definition forces you to compete on resolution, which favors high-field magnets. If the job is “resolution,” 7T always wins.
Level 2 (The Shift): “Diagnosing a stroke within the golden hour.”
Context: A stroke patient loses 1.9 million neurons per minute. The constraint is not image quality; the constraint is time. Driving the patient to the “Cathedral” takes 45 minutes. Bringing the scanner to the patient takes 5 minutes.
Level 3 (The Elevated Job): “Assessing neurological status at the point of care.”
The Acceptance Criteria: The job is not “make a pretty picture.” The job is “Binary Classification: Hemorrhage vs. Ischemia.”
The Implication: If a $50,000 low-res scanner can reliably distinguish blood (hemorrhage) from clot (ischemia) with 95% sensitivity, the “Resolution” metric is irrelevant. Diagnostic Sufficiency > Optical Perfection.
Path A: The Optimization Trap (Sustaining Innovation)
Path A engineers focus on “Helium-Free” 1.5T magnets (sealed systems like Philips BlueSeal).
The Logic: “Let’s make the Cathedral slightly cheaper to run.”
The Failure: It ignores the Projectile Effect. A 1.5T magnet is still a lethal weapon that sucks oxygen tanks, scissors, and gurneys across the room at 40 mph. It still requires a dedicated, access-controlled “zone.” It does not solve the access problem; it only solves the maintenance problem.
Path B: The Disruptive Deletion (Computational MRI)
Path B accepts Low Field Strength (e.g., 0.064 Tesla) as the constraint to unlock total mobility.
The Deletion: Delete the Cryostat. Delete the Quench Pipe. Delete the Copper Cage.
The Trade-off: Raw physics signal drops by a factor of ~400x compared to a 3T machine.
The Solution: Substitute Deep Learning for the missing signal.
The Result: A scanner that fits through a standard door, plugs into a wall outlet, requires no exclusion zone, and democratizes the “job” of neurological assessment.
Part IV: The Reconstruction (Physics & Code)
How do we reclaim the 42x efficiency gap? We rebuild the system using First Principles of electromagnetism and information theory.
Physics of the Halbach Array (The Zero-Power Magnet)
Instead of a solenoid (coil) that requires massive current to generate a field, we use a Halbach Array. This is a geometry of permanent magnets discovered by Klaus Halbach in the 1980s for particle accelerators.
Configuration: A specific arrangement of permanent magnets where the orientation of the magnetic field rotates by 90 degrees from one element to the next.
The Magic: This geometry augments the magnetic field on one side (the patient bore) and cancels it on the other (the exterior).
Benefit 1 (Zero Opex): It is a permanent magnet. It requires zero electricity and zero helium to maintain the
\(B_0\)field.
Benefit 2 (Self-Shielding): Because the field cancels itself aggressively outside the bore, the “5 Gauss Line” (the safety perimeter) is virtually flush with the machine housing. You can weld metal 2 feet away while it scans.
The “Infinite Shield” (Active EMI Cancellation)
Standard MRI requires a Faraday Cage—a copper-lined room that blocks FM radio signals, which otherwise swamp the delicate MRI signal. At 64mT, the Larmor frequency is ~2.7 MHz. While this is below the FM radio band, other noise sources (switching power supplies, motors) are prevalent.
The Software Fix: Active Noise Cancellation (ANC) Instead of blocking noise with mass (copper), measure the noise and subtract it.
Sense: External antennas mounted on the cart monitor the ambient electromagnetic environment.
Invert: The system correlates the external noise with the signal received from the patient coil.
Subtract: Using adaptive filtering (e.g., Least Mean Squares algorithms), the noise is subtracted from the readout in real-time.
Result: The MRI operates in a chaotic ER, next to IV pumps and iPhones, without a dedicated room. The “Cage” is now code.
Deep Learning Reconstruction (DL-ESPIRiT)
Low-field MRI produces “noisy” k-space data. A traditional Fourier Transform results in a grainy, unusable image. This is where the “Bits” replace the “Atoms.”
The Problem: Low SNR and Under-sampling.
The Model: We utilize Convolutional Neural Networks (CNNs), specifically U-Net architectures or Variational Networks (VarNet).
The Training Loop:
Input: Low-Field (0.064T) noisy scan data.
Ground Truth: High-Field (3T) scan data of the same patient (paired datasets).
Loss Function: Structural Similarity Index (SSIM) + L1 Loss.
The Inference: The AI learns the statistical probability of anatomical structures. It effectively “denoises” the image, using the faint signal from the 0.064T magnet as the structural scaffold, and “hallucinating” the texture based on learned biological priors.
Authority Anchor: As demonstrated by the FDA-cleared Hyperfine Swoop, this approach yields clinical T1/T2/FLAIR images sufficient for acute stroke detection at 64mT.
Part V: Market Reality Check & Execution Strategy
While the First Principles derivation suggests a $50,000 price point is inevitable, we must audit the current market landscape to understand why this hasn’t fully happened yet.
The “Reality Check” Audit (2025/2026 Context)
The core technologies (Low-Field Physics + Deep Learning) are no longer theoretical—they are commercially available. However, the economic deconstruction has lagged behind the technical deconstruction.
Hyperfine (Swoop):
Technical Status: Validates the entire thesis. 64mT, portable, Deep Learning reconstruction. FDA cleared.
Economic Reality: Currently priced between $250,000 - $360k (approximate commercial pricing). This represents a “Premium Portable” strategy rather than a “Commodity Utility” strategy. The gap between the $50k physics floor and the $300k commercial price is pure margin capture and R&D amortization, typical of early market entrants.
Promaxo:
Status: Validates the “Office-Based” thesis but is restricted to a specific niche (Urology/Prostate). It proves that low-field (0.066T) is clinically viable for intervention but hasn’t reached general utility status.
Synaptive (Evry):
Status: Represents “Mid-Field” (0.5T) disruption. It eliminates the quench pipe (sealed system) but retains the “Suite” form factor, failing to achieve true mobility.
The Conclusion: The “Physics Floor” of $50,000 is real. The current market is pricing at $250k+ because early adopters (ICUs) have low price sensitivity compared to rural clinics. The true disruption will occur when a entrant forces the price down to the $50k hardware limit, commoditizing the scan itself.
Option to Explore: Clinical Validation
Hypothesis: A 64mT scanner can clinically differentiate Ischemic vs. Hemorrhagic stroke.
Business Case Question: “Is the image ‘good enough’ to change a treatment decision?”
Investment: Fund the prototype and the “paired scan” study (Patient gets Low Field + High Field).
The Value: Validating this option unlocks the Mobile Stroke Unit market—putting MRIs in ambulances. This is a niche, high-value entry point.
Option to Expand: The “Vitals” Monitor
Once the cost drops below $50k and the weight below 500kg, the MRI ceases to be a “scheduled procedure.” It becomes a continuous monitor.
The Pivot: Move from “Snapshot in time” to “Video of recovery.”
New Job: Monitoring Traumatic Brain Injury (TBI) patients in the ICU for swelling (edema) in real-time.
The Moat: High-field scanners cannot do this because they cannot be brought to the bedside. This creates a monopoly on “Time-Series MRI Data.” We are no longer competing with Siemens; we are competing with the bedside monitor.
The Future State: Automated Interpretation
The bottleneck shifts from acquiring the image to reading the image.
Constraint: L3 Radiologists are expensive ($300+/hr) and sleep at night. Rural hospitals often wait 4+ hours for a read.
The Solution: An AI Agent that sits on the edge device. It analyzes the scan immediately and flags “Suspected Hemorrhage” to the neurosurgical team.
The End State: The scanner is a utility. The diagnosis is a service. The “Cathedral” is demolished. The patient is scanned in the ambulance, diagnosed by the algorithm, and routed to the O.R. before they even arrive at the hospital.
Appendix: The Physics of Deletion
Why 0.064 Tesla?
Why not 0.1T or 0.5T? The choice of 64mT is a specific optimization of the Larmor Frequency (~2.75 MHz).
Tissue Contrast: At lower fields, T1 contrast dispersion actually improves for certain tissues.
SAR (Specific Absorption Rate): Heating of patient tissue scales with the square of the frequency. At 64mT, tissue heating is negligible, allowing for faster pulse sequences that would be dangerous at 3T.
Wave Length: At 3T, the RF wavelength is short (~26cm), causing dielectric shading artifacts (standing waves) in the body. At 64mT, the wavelength is long (~10 meters), meaning the RF field is incredibly homogeneous. We delete the need for complex $B_1$ shimming.
The Energy Audit
1.5T Scanner:
Idle Power: 20-30 kW (Cryocooler + Helium Compressor).
Scan Power: 60-100 kW.
Wall Plug: 480V, 3-Phase.
0.064T Scanner:
Idle Power: 50 W (Computer sleep).
Scan Power: 900 W (Standard outlet max).
Wall Plug: 110V, Standard Household.
The energy delta confirms the efficiency of the First Principles approach. We have deleted the energy required to fight thermodynamics.
If you find my writing thought-provoking, please give it a thumbs up and/or share it. If you think I might be interesting to work with, here’s my contact information (my availability is limited):
Book an appointment: https://pjtbd.com/book-mike
Email me: mike@pjtbd.com
Call me: +1 678-824-2789
Join the community: https://pjtbd.com/join
Follow me on 𝕏: https://x.com/mikeboysen
Articles - jtbd.one - De-Risk Your Next Big Idea
New Masterclass: Principle to Priority
Q: Does your innovation advisor provide a 6-figure pre-analysis before delivering the 6-figure proposal?